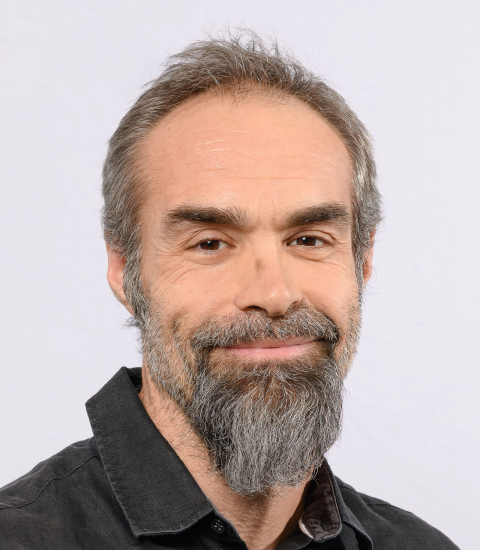
Biosketch
My research interest is focused on the interactions between the gut microbiome and the innate immune system in the context of various organ-specific autoimmune diseases.
During my PhD at the National Institute of Health and Medical Research (INSERM) in Unit 346 directed by Pr. Daniel Schmitt, I was focused on the influence of Toxoplasma gondii on human dendritic cells (DCs). We identified that this parasite has developed various strategies to regulate human DC function and escape immune response.
My post-doctoral training (from 2006 to 2011) was performed at the INSERM Unit 561 directed by Pr. Christian Boitard. My postdoctoral project was to investigate the role of DCs upon viral infection in a mouse model of autoimmune diabetes. We have demonstrated that a subset of DC (i.e., plasmacytoid DC (pDCs)) was central in the prevention of autoimmune diabetes conferred by viral infection. We demonstrated that virally-activated pDCs induced the expansion of regulatory T cells dampening the diabetogenic response in the non-obese diabetic (NOD) mice (J. Exp. Med 2011; Immunity 2009).
In 2011, I was appointed as permanent researcher at INSERM. I have initiated a project on the role of innate immune cells in the development of autoimmune diabetes in a non-infectious context in mice. We revealed an unknown mechanism of initiation of autoimmune diabetes, and we showed the unidentified role of neutrophils in autoimmune diabetes in mice (Nat. Med. 2013). This study represents an important step required for the future design of original clinical approaches based on the manipulation of innate immune cells in the prevention of autoimmune diabetes.
In 2013, I established my research group in the Institut Necker Enfants Malades (INEM) and I initiated an original project related to the role of antimicrobial peptides in autoimmune diabetes. We demonstrated that pancreatic endocrine cells under the control of the gut microbiota, expressed antimicrobial peptides preserving the immune tolerance in the pancreas (Immunity 2015, Cell Metab. 2018). Recently we showed the role of a specific intestinal antimicrobial peptide in the construction of a healthy gut microbiota in newborn mice and whether a defect in the expression of this peptide participates in the development of autoimmune diabetes. We further showed that antimicrobial peptide-expressing probiotic is an efficient strategy to correct the gut microbiota and prevent the development of autoimmune diabetes and potentially other dysbiosis-related diseases (Gastroenterology 2022). Our current projects aim to explore the crosstalk between the gut microbiota, the innate immune system, and non-immune cells in the context of autoimmunity and beyond and how antimicrobial peptides serve as messengers in this crosstalk and can be used as therapeutic tools.